CMS Health Equity Index: What every health plan needs to know now
Now is the time for Medicare Advantage health plans to understand how the new CMS Health Equity Index will impact future performance and reimbursement models. Wondering how this new initiative works? Don’t worry. We can help.

What is the HEI?
The Health Equity Index (HEI) is the latest in CMS’s commitment to driving improved health outcomes in socially vulnerable communities. The HEI will incentivize health plans to provide high-quality care and outcomes to their at-risk members. While CMS intents to add additional risk factors in the future, the initial HEI risk factors are below. CMS considers members who fall into the categories below as socially vulnerable and will include them in the HEI:
-
- Members receiving a low-income subsidy
- Members who are dually eligible for Medicare and Medicaid
- Members with a disability (those with a disability and/or end-stage renal disease as the original reason for entitlement to Medicare under age 65).
What’s the goal?
The CMS Health Equity Index (HEI) is a composite of several existing Star Rating measures. The HEDIS claims-based measures included in the calculation of the HEI are listed in the table below. This means that while none of the measures are new, the HEI is a new way to look at them together. CMS also plans to add other measures; however, they haven’t yet announced how they will do so. Using the HEDIS claims-based measures below allows health plans to get a good idea of their HEI score.
The HEI shows health plans’ performance across key measures among their most socially at-risk populations. CMS’s goal with the HEI is to incentivize health plans to perform well for their most vulnerable members. 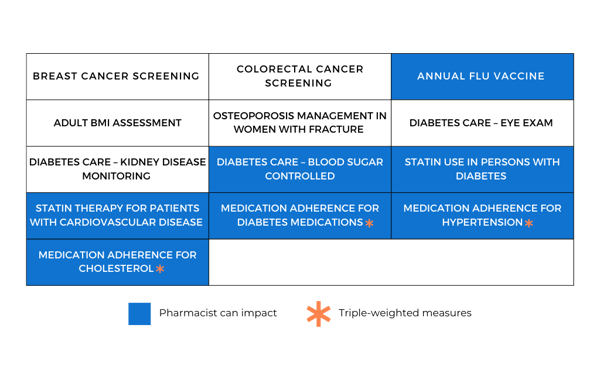
How to calculate the CMS Health Equity Index
First: Health plans are measured against their peers in each measure listed above for members with one or more social risk factor and divided into the top third, middle third, and bottom third by measure.
Second: Health plans in the top third of each measure receive one point, middle third plans receive no points, and bottom third plans lose a point.
Third: The HEI is calculated by taking the sum of all the index scores and dividing by the weighted number of measures (reminder: some measures are weighted higher than others). Because proper adherence to medications plays such a critical role in maintaining health, the three medication adherence measures listed above are triple-weighted. This means plans will receive +3, 0, or –3 points for each adherence measure.
Finally: The HEI score is multiplied by a reward factor of 0.4, and the resulting number is added to the health plan’s Star Rating. For example, a 4.3 Star plan with an HEI of 0.5 would be upgraded to a 4.5 Star plan (0.5 HEI x 0.4 reward factor = 0.2), which would put the plan into the next highest bracket.
Implementing change takes time, but we can help
The new CMS Health Equity Index is coming sooner than many health plans realize. Beginning in 2027 CMS will begin calculating HEIs using health plan data from 2025 and 2026.
There are only a few years to get your health plan’s clinical programs up and running to ensure you’re serving your most vulnerable members and getting the maximum benefit from the new HEI. Luckily, the experts at Aspen RxHealth can help you along the way.
The good news is that pharmacist-led clinical programs make a direct impact on the most highly weighted HEI measures. That’s because pharmacists can be the key to empowering members to take a more active role in their health. There are nearly countless ways for pharmacists to improve health outcomes for the most socially at-risk members. These include boosting medication adherence, educating about the benefits of routine vaccinations, or counseling on medication interactions.
No matter if you have in-house pharmacists and need an end-to-end technology solution, or you’re looking to tap into the power of over 7,000 Aspen RxHealth remote pharmacists, we’re ready and able to help serve health plans just like yours.
Reach out to us at aspenrxhealth.com/contact to learn more about the Health Equity Index and speak with a member of our team.